Did you know that diabetes-related eye disease is one of the leading causes of preventable blindness in the U.S.?
Yet, most people living with diabetes don’t realize how quietly and dangerously it can affect their vision.
If you’ve been managing your blood sugar, taking your medications, and watching your diet, you might feel like you’ve got everything under control. But there’s a piece many patients overlook until it’s too late: their eyes.
Diabetes doesn’t just impact your energy levels or your heart. It changes the way blood flows through tiny vessels in your eyes, sometimes without warning, and those changes can lead to vision loss or even permanent blindness.
But here’s the good news: up to 90% of diabetes-related vision loss is preventable with early detection and proper care.
Let’s walk through it together.
What Is Diabetic Eye Care?
Diabetic eye care is a specialized form of eye health management explicitly designed for people with diabetes. It focuses on the early detection, prevention, and treatment of eye complications caused by fluctuations in blood sugar levels.
It includes:
- A comprehensive dilated eye exam every year (minimum)
- Ongoing monitoring for early signs of damage
- Coordinated care with your primary doctor or endocrinologist
- Fast action when signs of trouble appear
This isn’t just a routine check-up; this is essential protection for one of your most important senses.
According to a study, about 1 in 3 people with diabetes over age 40 already has diabetic retinopathy, the most common form of diabetes-related eye disease. And many don’t even know it yet.
What Is Diabetic Eye Disease?
Diabetic eye disease refers to a group of eye conditions that stem from diabetes. The most common include:
- Diabetic retinopathy
- Diabetic macular edema (DME)
- Cataracts
- Glaucoma
Each of these conditions affects vision differently. Some damage blood vessels. Others increase fluid pressure in the eye or cloud your lens. But they all have one thing in common: they’re linked to blood sugar control.
Diabetic Retinopathy: A Silent Vision Thief
Diabetic retinopathy is the leading cause of vision loss in working-age adults in the U.S. It affects nearly 8 million Americans, and that number is expected to roughly double by 2050.
It occurs when high blood sugar damages the tiny blood vessels in your retina. At first, you may not notice anything at all. But behind the scenes, those vessels may start to swell, leak, or close off entirely.
Over time, abnormal new blood vessels may form, but they’re weak, and they can bleed into the eye or even cause retinal detachment.
Two Stages of Diabetic Retinopathy:
- Nonproliferative (NPDR): Early-stage; blood vessels weaken and leak.
- Proliferative (PDR): Advanced stage; new vessels form, increasing risk of severe vision problems.
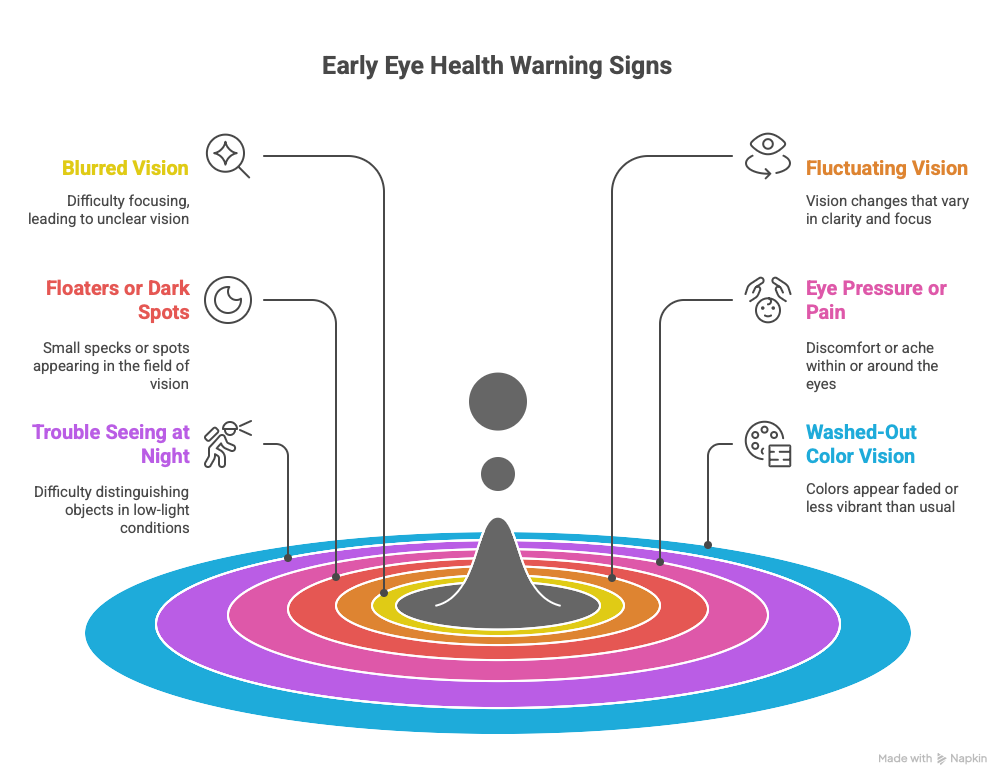
Warning Signs to Watch:
- Blurred or fluctuating vision
- Eye floaters or dark spots
- Difficulty seeing at night
- Vision that changes with your blood sugar
The problem? Most people don’t feel or see symptoms until serious damage has occurred, which makes regular diabetic eye care essential.

Diabetic Macular Edema (DME): The Hidden Swelling
Diabetic macular edema is a complication of diabetic retinopathy. It’s caused by fluid leaking into the macula, the central part of your retina that helps you read, drive, and recognize faces.
Why It Matters:
- DME affects about 750,000 Americans.
- It’s the primary cause of vision loss in diabetic retinopathy.
- It can happen at any stage, even without noticeable symptoms.
Common Symptoms:
- Wavy or blurry central vision
- Washed-out colors
- Trouble reading or seeing fine details
With regular eye exams, DME can often be caught early and treated with medications or laser therapy to preserve vision.
Diabetes and Cataracts: Clouding Up Early
Cataracts are a natural part of aging, but diabetes speeds things up. Diabetics are 2 to 5 times more likely to develop cataracts and often get them at a younger age.
What Happens:
The lens inside your eye becomes cloudy, making your vision blurry, foggy, or dim.
Symptoms:
- Trouble with bright lights or glare
- Colors look faded
- Double vision in one eye
- Needing frequent prescription changes
Thankfully, cataracts can be removed through safe and effective surgery. But prevention through blood sugar control and regular diabetic eye care is key to delaying surgery as long as possible.
Maintaining good corneal and lens health through proper nutrition may help delay cataract development. Explore the top foods that support eye health and corneal strength.
Diabetes and Glaucoma: Pressure That Builds Silently
Glaucoma is a group of conditions that damage the optic nerve, often caused by increased pressure inside the eye. People with diabetes are twice as likely to develop glaucoma.
Symptoms (Often Silent at First):
- Gradual loss of side (peripheral) vision
- Tunnel vision (in advanced stages)
- Eye pain or pressure (less common)
Because it often progresses without symptoms, glaucoma can go unnoticed until vision loss is permanent. Early detection through eye pressure checks and optic nerve exams can stop it in its tracks.
Other Vision Problems Linked to Diabetes
Even without a diagnosed eye disease, diabetes can still impact your vision temporarily — especially when blood sugar is unstable.
Common Vision Effects:
- Blurry vision: Rapid changes in blood sugar can temporarily distort your lens shape.
- Double vision: Nerve damage can affect how your eyes move.
- Shifting focus: Difficulty adjusting your eyes between near and far.
These changes often improve with better glucose control, but they’re another reason why consistent diabetic eye care is vital.
Who’s Most at Risk?
Certain factors make it more likely that diabetes will affect your vision:
- Long-standing diabetes (10+ years)
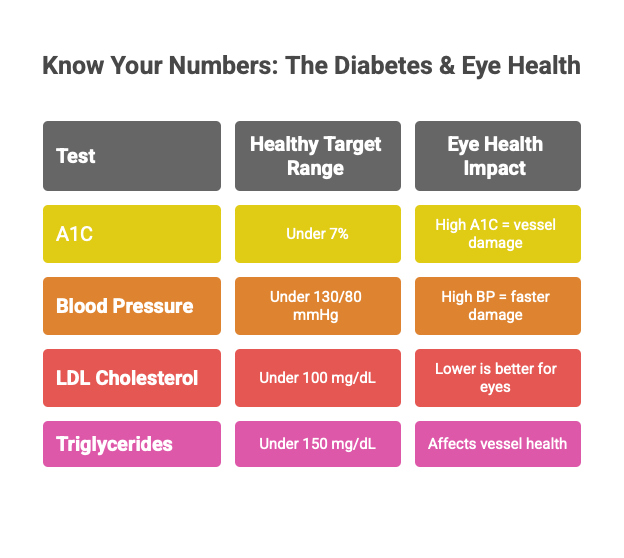
- Poor blood sugar control (high A1C levels)
- High blood pressure or cholesterol
- Kidney disease
- Pregnancy (gestational diabetes or type 1/type 2)
- Smoking
- Family history of diabetic eye disease
If any of these apply to you, it’s even more important to stay on top of your diabetic eye care routine.
What Does a Diabetic Eye Exam Involve?
Your eye doctor will do more than just check your glasses prescription.
A complete diabetic eye exam includes:
- Dilated pupil exam to look at the retina and blood vessels
- OCT scan (Optical Coherence Tomography) to detect swelling
- Fluorescein angiography to identify leaks or new vessel growth
- Eye pressure test to screen for glaucoma
This exam is painless, quick, and could prevent permanent vision loss.
Treatment Options: What Happens If Something’s Found?
If your eye doctor spots signs of diabetic retinopathy, DME, or another condition, don’t panic. There are effective treatment options:
- Anti-VEGF injections (like Eylea or Lucentis) to stop vessel growth and reduce swelling
- Laser treatments to seal leaking blood vessels or prevent bleeding
- Vitrectomy surgery to remove blood or scar tissue
- Prescription eye drops (for glaucoma) to reduce pressure
- Cataract surgery to restore clear vision when lenses become clouded
Early treatment leads to better outcomes. That’s why acting quickly is so important.
7 Ways to Protect Your Eyes (Starting Now)
- Get your annual dilated eye exam no matter what.
- Control your blood sugar (target A1C < 7%) to prevent vessel damage.
- Manage blood pressure and cholesterol — both affect your eyes.
- Eat a vision-friendly diet rich in greens, berries, fish, and whole grains.
- Exercise regularly to improve blood flow and glucose stability.
- Avoid smoking, which worsens blood vessel damage.
- Communicate with your care team to coordinate between your eye doctor, PCP, and endocrinologist.
Don’t Wait for Symptoms to Take Action
Your eyes are your connection to the people, places, and moments that matter most. Whether it’s watching your kids grow, driving to work, or simply enjoying a sunset, your sight is worth protecting.
At Center For Sight Southwest Florida, we understand the unique challenges of diabetic eye care. Our team utilizes advanced diagnostic tools, personalized treatment plans, and a patient-first, warm approach to help you protect your sight.
If you have diabetes and haven’t had an eye exam in the past year, it’s time. Let’s not wait for symptoms. Let’s stay ahead of them.
Contact us today to schedule your diabetic eye exam.
Frequently Asked Questions
1. Can diabetic eye disease be reversed?
Many people wonder if vision lost to diabetic eye disease can be restored. While early detection and treatment can prevent further damage and sometimes improve vision, advanced damage is often permanent. This is why regular eye exams and prompt treatment are so crucial.
2. How often should I get my eyes checked if I have diabetes?
It’s recommended to have a comprehensive dilated eye exam at least once a year. However, if you already have signs of diabetic eye disease or other risk factors, your doctor may suggest more frequent exams (every 2–4 months in some cases).
3. Are there warning signs I should watch for between eye exams?
Diabetic eye disease often develops without noticeable symptoms. However, see your eye doctor promptly if you notice sudden vision changes, new floaters, flashes of light, blurred or patchy vision, or difficulty seeing at night.
4. Does good blood sugar control guarantee I won’t get diabetic eye disease?
Good blood sugar control significantly lowers your risk, but it doesn’t eliminate it entirely. Other factors, such as blood pressure, cholesterol levels, duration of diabetes, and genetics, also play a role.
5. Are diabetic eye exams different from regular eye exams?
Yes. Diabetic eye exams include a dilated retinal exam and often advanced imaging (like OCT or fluorescein angiography) to detect subtle changes that may not affect vision yet.
6. Is diabetic eye disease painful?
Most diabetic eye conditions are painless in the early stages. Pain is uncommon, but if you experience eye pain, pressure, or sudden vision loss, seek medical attention immediately.
7. Can children or young adults with diabetes get diabetic eye disease?
Yes, anyone with type 1, type 2, or gestational diabetes is at risk, regardless of age. The risk increases the longer you have diabetes.
8. What happens if I’m pregnant and have diabetes?
Pregnancy can increase the risk and speed of progression of diabetic eye disease. It’s important to have an eye exam before pregnancy or early in the first trimester, and possibly more frequently during pregnancy.
9. Will my insurance cover diabetic eye exams and treatments?
Most health insurance plans, including Medicare, cover annual diabetic eye exams and many treatments when medically necessary. Check with your provider for details.
10. What lifestyle changes can help protect my eyes beyond blood sugar control?
Managing blood pressure and cholesterol, eating a healthy diet, exercising regularly, avoiding smoking, and keeping regular appointments with your healthcare team all help protect your vision.



